1. The main purpose of animal testing
The main purpose of animal testing of medical devices is to study the safety of medical devices. Often the subject of animal testing in medical research may be a new diagnostic method and principle, or the mechanism of action of a new drug, etc. Its main purpose is to study the mechanism, effectiveness and safety of the device. Its main research objectives are mechanism, efficacy and safety. This research may or may not be linked to the use of a medical device. The study may or may not involve materials that are implanted or in contact with the body's circulatory system.
The ability to establish a well-conforming animal model during the study is critical to the success of the trial. There are, of course, often situations where it is not possible to establish a suitable animal model for testing. Whether or not to establish a well-conforming animal model in animal testing of medical devices depends on the objective conditions and the purpose of the study.
2. Key elements of animal testing
When an animal test model is established appropriately, the study of effectiveness can be an important element of animal testing of medical devices. That is, the conformity of the actual use of the test device to its intended use. However, the results of such studies cannot be used as objective evidence for the evaluation of the effectiveness of a medical device and can only be used as an auxiliary reference for whether it can be transferred to humans for clinical studies. It can also be an input and output information for studies on the mechanism of diagnostic and therapeutic action.
Objective studies of effectiveness are not possible if, in animal testing, no matter how you design the animal model, it differs significantly from the human subject for which the device is intended, or if the cost of designing and completing an animal model that matches or approximates the intended use of the human subject is too great, or if it is influenced by animal protection forces. In most cases, it is not practical to verify the effectiveness of a medical device in animal testing.
3. Triality evaluation of animal testing
In animal testing there is a triple evaluation of physical, chemical and biological properties. In the physical evaluation, such as the rigidity, elasticity, energy and fatigue properties of the device material due to the great differences between animal subjects and humans in terms of weight, volume, activity, muscle density, bone strength, etc.. And these properties may be important technical characteristics of the device and are one of the components of the effectiveness of the product. For example, bone studs, artificial joints, etc. It is therefore not possible to verify the clinical effectiveness of the device under test by animal testing.
In comparison, chemical evaluation is relatively clear, objective, easy to grasp and operate. For example, chemical evaluations are generally carried out on residual monomers, harmful metal elements, various additives, etc. in materials.
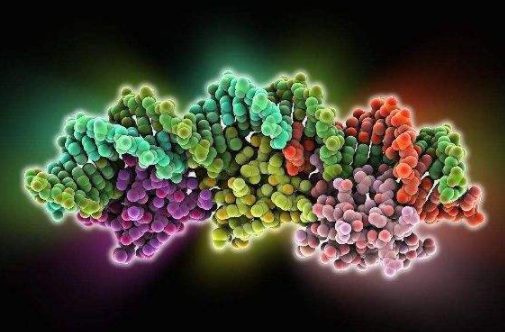
Biological evaluations, on the other hand, focus on acute toxicity tests, allergenicity tests, long-term implantation tests, cytotoxicity tests, genotoxicity tests, as well as carcinogenicity tests and immune rejection tests. Although the conclusions of such evaluations are also subject to discrepancies with humans and the release of residues or degradation products that cannot be determined and controlled. There is also bias in the evaluation results, interference from confounding factors, etc. However, biological compatibility testing has been able to reach the organ, tissue, cellular and even molecular level, and help in deciding whether or not it can be transferred to humans for clinical trials can be evident.
4. The importance of animal testing for medical device safety
We all know that one of the purposes of animal testing is the verification of safety. Biocompatibility itself is one of the safety features of a device. The difference is that animal testing of implantable medical devices involves the observation and evaluation of the above-mentioned tests after the implantation of the device material directly into the animal in the appropriate location.
Biological compatibility tests and evaluations are generally carried out by injecting a test solution and a blank control solution into the test animal with the device material under test. The latter is therefore closer to the objective reality for implantable materials. The use of the former method alone prior to the first clinical study of an implantable device carries a high degree of risk for the subject.
Once the animal tests have been passed, it can be said that the biocompatibility tests and evaluations have also been passed. In this way, the purpose of animal testing prior to clinical trials of implantable medical devices for the first time in humans is the same as that of biological evaluation prior to clinical trials of medical devices. However, the objectives and conclusions of animal testing are broader and more objective.
There are many items in animal testing that cannot be included in biocompatibility testing. Biocompatibility testing cannot be used as a substitute for animal testing for first time implantable devices. Therefore, to use a first implantable device directly in a clinical study without animal testing instead of biocompatibility testing would be extremely irresponsible to the subjects who will be involved in the clinical trial.
Of course, due to the large number of uncontrollable factors involved in animal testing and biocompatibility testing. This, coupled with the differences between animal models and human responses, as well as the individuality of the human body itself, makes animal testing and biocompatibility testing very limited.
It is therefore the clinical research phase of a medical device that is the key stage in its validation of effectiveness and another stage in the verification of safety. Human differences vary in their tolerance to, for example, implantable materials, radiation doses, etc. Clinical trials take into account the effects of differentiation to ensure that the risk of its clinical use is at an acceptable level for all user groups.