Microscopic examination has been the standard method for malaria diagnosis for a century. However, the huge workload combined with the lack of professional staff leads to a not-so-low misdiagnosis rate. Misdiagnosis or delayed diagnosis of malaria can have serious consequences for patients.
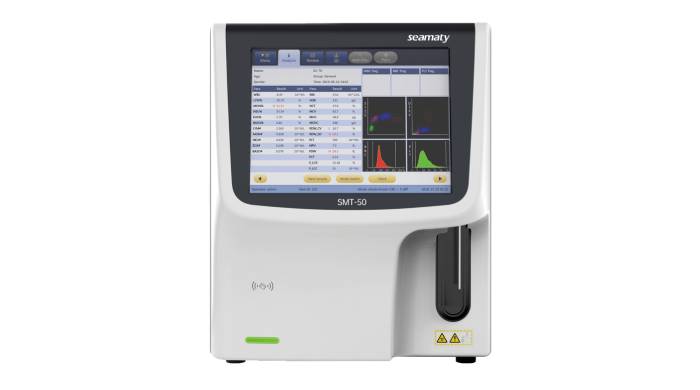
In the last decade or so, efforts have been made to use fully automated blood analyzers for malaria diagnosis. However, the accuracy of malaria diagnosis varies depending on the test method, immunoclinical background, and parasite load or species. Future developments in new hematology analyzers, such as simplified, enhanced, or inexpensive alarm-equipped malaria detection devices, will greatly increase the overall detection capacity of the instrument. This will also expand the role of hematology analyzers in clinical diagnostics.
Hematology analyzers currently being investigated for malaria blood diagnosis include the Coulter series, Abbott Cell-Dyn, and Sysmex's XE/XN series. However, none of them has a complete testing system for malaria.
The Abbott Cell-Dyn series of hemocytometers can test for malaria pigments (hemoglobin). It works by detecting cell characteristics through different channels to classify different cells.
-
x-axis: 90 degree lateral scatter,.
-
y-axis: 90-degree depolarized lateral scatter.
-
Blue scatter is for lymphocytes; purple scatter is for monocytes; orange scatter is for neutrophils; green scatter is for eosinophils.
-
The purple arrows point to cells containing heme in P. falciparum patients. The black scattered dots pointed by the black arrow are the cells containing hemoglobin in P. falciparum patients. The cells that the arrows point to are all theoretically Plasmodium.
Compared to the scatter plot of P. falciparum, the scatter plot of P. falciparum does not differ much from the scatter plot of normal samples, except that there are a few protruding scatters in the area of monocytes (purple scatters).
For the Sysmex XN series blood analysis system, malaria blood samples were analyzed by WNR (nucleated leukocyte) channel and WDF (white blood cell differential) channel.
In the WNR channel, the hemolytic agent will lyse the parasitic red blood cells, so the parasitic red blood cells will show a lower FSC, but a higher SSC and SFL, so the parasitic cells can be shown separately in the scatter plot.
In the WDF channel, incomplete lysis of erythrocytes by the WDF hemolysate. Thus parasites within the erythrocytes would theoretically result in additional fluorescence.
Of course there are still significant limitations to hematology analyzer screening for malaria. For example with very low parasite loads they are more likely to overlap with cellular debris in the scatter plot and do not form separate scatter clusters like other blood cells. But the introduction of blood cell analyzers as a tool for the diagnosis of malaria may have great practical importance in the long run.
Rapid screening of suspected patients by automated hematology analyzers remains uniquely present compared to current commercially available malaria testing methods. Automated hematology analyzers have great potential. New blood cell analyzers will be available one after another as the analyzer's detection capability is updated. It is believed that the diagnosis of malaria can be solved in the near future.