release time:2024-05-24 14:50:07
Blood gas analysis is a critical diagnostic tool used to evaluate respiratory function, acid-base balance, and metabolic status in real-time, reflecting the patient's current condition. It aids in clinical monitoring and treatment adjustment across various medical fields.
But what exactly is blood gas analysis and how does a blood gas analyzer work? What are its clinical implications, common parameters, and application scenarios? Let’s explore these aspects together.
Blood gas analysis involves a comprehensive examination of various gases and acidic or basic substances in the blood, with common indicators including partial pressure of oxygen (pO2), partial pressure of carbon dioxide (pCO2), and pH levels. Broadly, it also includes analysis of electrolytes, lactate, glucose, and their derivatives.
This analysis is vital for managing respiratory failure due to pulmonary diseases, critical care, internal medicine, surgery, obstetrics, pediatrics, shock, major burns, and surgical procedures. It is now widely used in clinical departments of hospitals.
The primary clinical significance of blood gas analysis is to assess respiratory function and acid-base balance in the body. It helps:
|
Parameter |
Description |
Reference Range |
|
pH |
Indicates blood acidity or alkalinity. Arterial pH < 7.35 indicates acidosis, and > 7.45 indicates alkalosis. Normal pH does not always mean there is no acid-base imbalance; other indicators should be considered. |
7.35-7.45 |
|
pCO2 |
Reflects alveolar ventilation efficiency. |
35-45 mmHg |
|
pO2 |
Indicates oxygen partial pressure in the blood. |
83-108 mmHg / 11.1-14.4 kPa |
|
Na+ |
Essential for extracellular fluid volume, osmotic pressure, acid-base balance, and cellular function. |
138-146 mmol/l |
|
K+ |
Main cation for cellular activity; important for maintaining normal osmotic pressure, acid-base balance, glucose and protein metabolism, and neuromuscular function. High levels can cause arrhythmias. |
3.5-4.9 mmol/l |
|
Ca2+ |
Vital for neuromuscular excitability, gland secretion, and enzyme activity. |
1.12-1.32 mmol/l |
|
Cl- |
Major extracellular anion; useful in differentiating types of metabolic acidosis. |
98-109 mmol/l |
|
Glu (Glucose) |
Essential nutrient for metabolism. |
3.9-5.8 mmol/l |
|
Lac (Lactate) |
Elevated levels indicate reduced blood perfusion or tissue hypoxia. |
0.36-1.25 mmol/l |
|
Hct (Hematocrit) |
Percentage of red blood cells in blood; impacts blood viscosity and reflects red cell mass. |
38-51% |
|
HCO3- (Bicarbonate) |
Indicates actual bicarbonate content in the blood; crucial for acid-base balance. |
21-28 mmol/l |
Emergency Resuscitation: In emergency settings, patients often experience metabolic imbalances. Rapid acquisition of blood pH, pO2, and pCO2 values is essential for correcting acid-base imbalances and effectively resuscitating patients.
Blood gas analysis is indispensable in clinical practice, offering critical insights for diagnosis, treatment, and prognosis. Its reports provide robust evidence for clinical decisions and help prevent medical disputes through evidence-based practice.
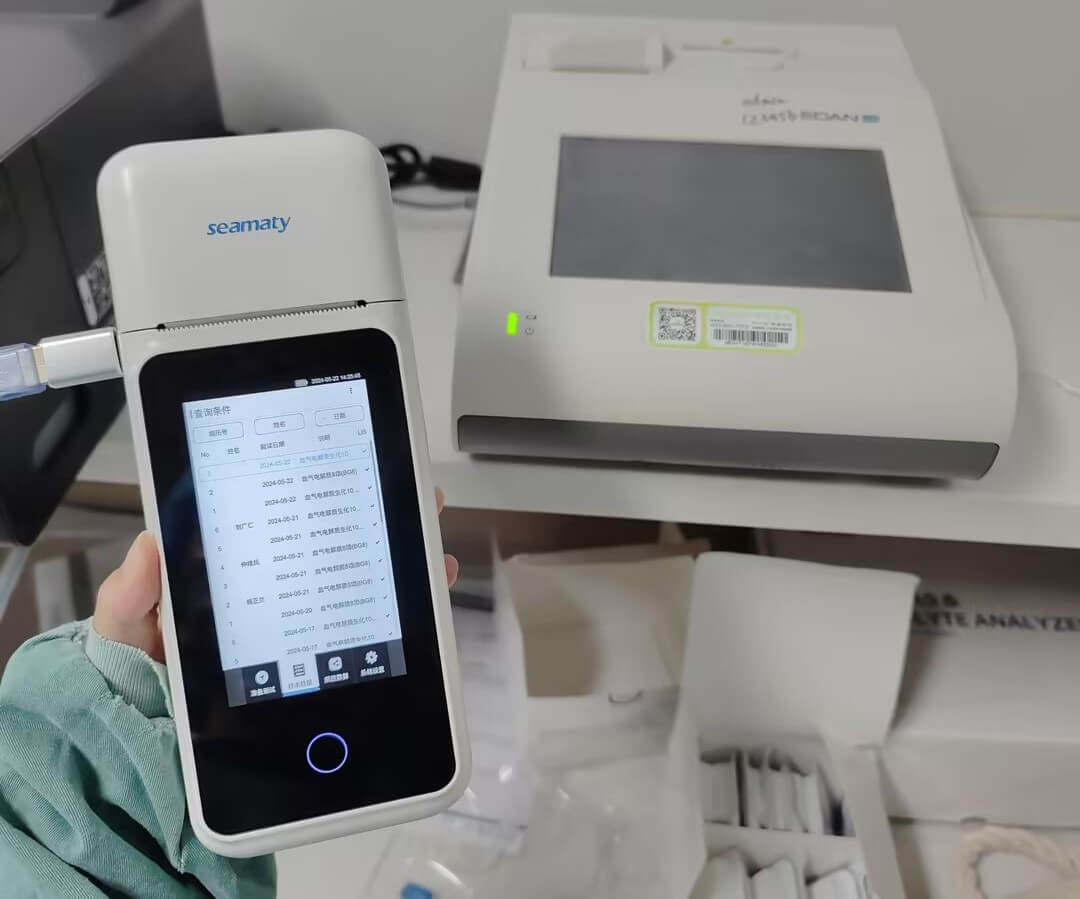
- Portable and efficient: Handheld operation with results in three steps.

The Seamaty SG1 uses biosensing, microfluidics, reagent embedding, and other technologies, condensing complex blood gas analysis into a device the size of a POS machine. Its compact size and built-in large-capacity battery expand its usage scenarios beyond laboratories to bedside, clinics, emergency rooms, ambulances, and field hospitals, aiding doctors in making rapid treatment decisions.

2024-09-19
Upgrade your clinical testing capabilities with the Seamaty SMT-70 Semi-auto Chemistry Analyzer. Affordable, compact, and user-friendly, it delivers reliable results with minimal maintenance. Ideal for labs seeking budget-friendly, efficient solutions.
2022-09-12
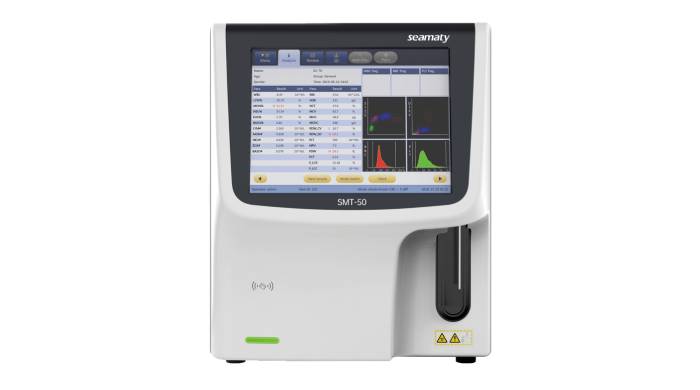
Hematology is a branch of medical science that deals with the study of blood, blood-forming organs and diseases. Hematology analyzers are an important part of this field, used to diagnose and monitor conditions like leukaemia, anaemia and sickle cell disease. If you're interested in learning more about hematology analyzers, or want to know which one is best for your needs, read on.
2022-07-25
The biochemistry field of study is vast and complex. It is constantly evolving as scientists uncover new information about the way that cells work. A key part of any biochemistry lab is the auto analyzer tool.