Biochemical testing requires the collection of patient's blood, but the quality control before biochemical testing is an important link, but also the most easily ignored link. According to incomplete statistics, errors caused by factors prior to biochemical analysis account for more than 70% of experimental errors.
In this paper, we elaborate on 3 aspects: patient preparation before biochemical blood sample collection, requirements for health care personnel in venous blood collection and specimen transport reception.
1. Preparation of patients before blood sample collection
-
1) Avoid strenuous exercise: strenuous muscle exercise obviously affects the body's metabolism and causes changes in the concentration of certain components in the blood. For example, elevation of lactate, creatine kinase (CK), aspartate aminotransferase (AST), lactate dehydrogenase (LDH), alkaline phosphatase (ALP), glucose (GLU), etc. Therefore, it is generally recommended to refrain from strenuous exercise for 24 hours before blood sampling, preferably in the early morning. Inpatients can have their blood taken before they wake up. Patients who are rushed to the outpatient clinic should take blood after at least 15 minutes of rest.
-
2) Pay attention to a reasonable diet: Except for emergencies or other special reasons, it is generally advocated to take blood on an empty stomach after 12 hours of fasting. Prolonged fasting (starvation) or post-meal changes in the chemical composition of the blood can cause changes. For example, blood glucose and protein decrease and bilirubin increases during starvation. Postprandial blood glucose, blood potassium, alkaline phosphatase and triglycerides usually increase, inorganic phosphorus decreases, and serum may be cloudy.
-
In addition, the amount of diet has an effect on the test results. For example, a high protein diet may increase serum urea, ammonia, and uric acid. A high-fat diet causes celiac disease, resulting in cloudy serum. Drinking too much or too little water can make the blood dilute or concentrate. Caffeinated beverages can cause the release of catecholamines, etc. The components of blood that are affected by diet and have a large variation include potassium ion (K+), GLU, total cholesterol (TC), triglycerides (TG), inorganic phosphorus (IP), etc.
-
3) Avoid drinking alcohol before blood sampling. Drinking alcohol before blood collection can cause a rapid increase in blood lactate and uric acid. Continuous alcohol consumption can make AST, alanine transaminase (ALT), γ-glutamyl transferase (γ-GT) rise, while γ-GT rises most significantly. Chronic alcohol drinkers often have triglyceridemia and γ-GT can be chronically abnormal.
-
4) Avoid tension and emotional excitement. Otherwise, it may affect the neuroendocrine function, affect respiration, and make lactic acid and other elevated.
-
5) The effect of body position when taking blood. Changes in body position (standing, sitting, lying) can cause significant changes in certain test indicators. Therefore, it is recommended that blood be taken after 5 minutes in a sitting position.
-
6) Avoid the influence of drugs. Many drugs (hormones, hypoglycemic drugs, diuretics, antiepileptic drugs, anti-cancer drugs, etc.) into the body can make some test results higher or lower. When analyzing and judging biochemical test results, we should pay attention to the history of drug use.
2. The requirements of the medical personnel for venous blood collection
-
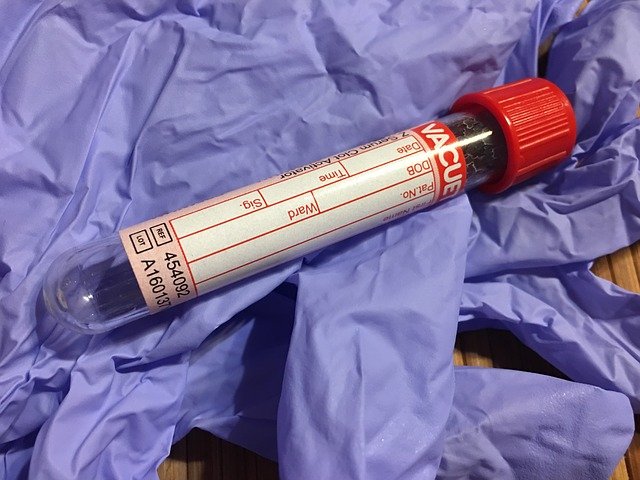
1) the correct use of anticoagulants. Usually clinical biochemical tests mostly use serum as specimens. Some special tests require the use of anticoagulants, should pay attention to the selection of appropriate anticoagulants and pay attention to the ratio of anticoagulants to blood. This is to prevent specimens from hemolysis or changes in the morphology of red blood cells. Immediately after blood collection, shake well to prevent clotting.
-
Commonly used anticoagulants are heparin and EDTA-K2. heparin is mainly used for blood gas, blood ammonia, lactate, and emergency biochemical determinations. EDTA-K2 is used for troponin and glycated hemoglobin determinations. If drawn into other anticoagulation tubes not drawn into green cap tubes or red cap tubes, do not pour the blood back into green cap tubes or red cap tubes. The blood should be redrawn. Because this will seriously affect the results of K+, Ca2+ assay.
-
2) Pay attention to the order of blood collection. When using vacuum blood collection tubes, blood should be collected in the following order: coagulation tubes, blood sedimentation tubes, blood routine tubes, heparin tubes, then other anticoagulation tubes, and finally non-anticoagulation tubes. If blood culture is done then the culture bottle specimen is taken first to prevent contamination.
-
3) The correct way to shake and mix. Immediately after blood collection, turn upside down and mix 5 to 8 times. Do not move violently.
-
4) Blood should be protected from direct sunlight. Prevent substances such as bilirubin and uric acid that are sensitive to ultraviolet light from decomposing due to exposure.
-
5) The specimen should be sent for testing in time after collection. Otherwise, due to the metabolism of blood cells, gas exchange and transfer of substances to make changes in a variety of components inside and outside the blood cells, resulting in errors in the analysis results.
-
6) The amount of specimens collected should ensure the needs of monitoring and retesting. After collection, the serum should be separated promptly and tested as soon as possible. Separation of serum or plasma should be centrifuged according to the centrifugation time and speed required by the operating instructions of each project. The laboratory temperature should be maintained at 15 to 30°C. And should be covered to prevent evaporation of specimen moisture and specimen concentration.
3. Transport and receipt of samples
Nurses of clinical departments and outpatient laboratory personnel are responsible for the collection of specimens. A corresponding barcode is placed on the container in which the specimen is collected. Nurses, nurse practitioners or trained field personnel are responsible for specimen delivery. The biochemistry team of the laboratory department is responsible for the receipt, testing and storage of specimens for processing.
Rejection principles for unqualified specimens.
1) Specimens sent for testing that do not meet the requirements for specimen collection and transportation (wrong category of vacuum tubes, coagulation of anticoagulated blood, large air bubbles, coagulated filaments, clots in specimens for blood gas analysis, specimens not sent for testing in a timely manner).
2) The test application form does not match the specimen.
3) specimen blood draw is not enough, not in line with the standard amount of vacuum blood collection tubes
4) Specimen hemolysis, jaundice, celiac disease must be contacted with the clinician. Depending on the clinical requirements for testing (hemolysis and celiac disease are indicated on the test sheet) or redrawing blood and re-measurement and marked on the test sheet.
5) The name and other information on the test sheet are not consistent with the barcode information on the specimen.
In summary, there are many factors affecting specimens before analysis, so we need to do a good job of communication and training with clinical staff to improve the pre-analytical management of biochemical samples.