In recent years, with improved nutrition and medical care, concern for the health of pets and an increase in the average life expectancy of pets, there has been an increase in various geriatric diseases. Diabetes is one of these.
Diabetes is a multi-causal metabolic disease characterised by chronic hyperglycaemia, accompanied by disorders of glucose, fat and protein metabolism caused by defects in insulin secretion and action. Diabetes causes chronic damage, dysfunction and failure of multiple organs.
Biochemical testing is increasingly recognised by clinical veterinarians as an aid to the diagnosis and treatment of diabetes in cats. This article will briefly discuss the changes in the biochemical parameters during the course of diabetes in cats.
1. Classification of diabetes mellitus
The pathogenesis of diabetes mellitus and the pathological changes in the pancreatic beta cells can be classified into type I and type II. However, this classification is of little relevance to the clinical management of diabetes mellitus. It is more meaningful to classify it as
1.1 Insulin-dependent diabetes mellitus
Also known as Type I diabetes, it is characterised by the destruction of beta cells, resulting in insulin deficiency. Complete loss of insulin secretion may occur and a lifelong need for insulin therapy. This type of diabetes is the most frequent form of diabetes, with almost 50-70% of affected cats having insulin-dependent diabetes.
1.2 Non-insulin-dependent diabetes mellitus
Also known as type II diabetes. It is characterised by insulin resistance and beta-cell dysfunction. Insulin secretion in this type of affected cat may be increased, decreased or normal compared to normal fasted animals. However, the amount of insulin is not sufficient to overcome insulin resistance in the peripheral tissues, resulting in relative insulin deficiency. Clinically this type of diabetes is most commonly seen in cats. It accounts for approximately 30-50% of all diabetes in cats.
1.3 Secondary diabetes mellitus
This type of diabetes is caused by extensive destruction of the pancreatic islets due to known diseases such as inflammation, tumours, surgery, or due to other endocrine diseases that affect the secretion or action of insulin. Examples include hyperthyroidism and abnormal secretion of growth hormone due to progesterone. These hormones counteract the action of insulin and cause insulin resistance.
2. Pathogenesis
2.1 Insulin-dependent diabetes mellitus
Immune damage is caused to pancreatic β-cells by the action of T-cells and antibodies. That is, oxygen free radicals and nitrous oxide from T cells and macrophages cause mitochondrial damage to β cells DNA disintegration leading to death. As a result beta cells and insulin secretion are almost completely lost immunity to cells of diseased animals with genetic susceptibility. Damage can be triggered by environmental factors such as viruses, toxins and exposure of young cats to exogenous antigens.
2.2 Non-insulin-dependent diabetes mellitus
This type of diabetes mellitus is most commonly seen in cats. Histology, clinical signs and laboratory data suggest that this type of diabetes in cats is similar to type II diabetes in humans.
The pathological mechanism is impaired β-cell function and abnormal insulin secretion in response to increased blood glucose. Several abnormalities in insulin secretion can lead to the development of the disease.
In the first stage insulin secretion is significantly reduced or absent. The mechanisms underlying the impairment of insulin secretion in type II diabetes are mostly based on laboratory studies. In order to stimulate insulin secretion, extracellular glucose must bind to receptors on pancreatic beta cells, which are receptors and transport carriers for glucose, followed by signals from intracellular glucose metabolism to cause insulin secretion. As a result, the ability of extracellular glucose to stimulate insulin is significantly reduced.
Another mechanism is that the body becomes resistant to insulin. Insulin resistance is defined as a significant reduction in the physiological effect of insulin secretion at normal levels to stimulate glucose uptake and utilisation by target cells. Alternatively, an extraordinary amount of insulin is required to maintain the normal physiological effects of glucose uptake and utilisation by target cells.
Skeletal muscle is the most important site where insulin resistance occurs, but other tissues, including the liver, can also produce insulin resistance. In skeletal muscle, insulin resistance reduces glycogen synthesis. In the liver, insulin inhibits gluconeogenesis and glucose release. The binding of insulin to receptors is rarely affected. The main cause of insulin resistance is a post-receptor defect.
Due to post-insulin receptor defects in insulin target cells, nutrients are not well utilised once they enter the cells, which in turn produces hyperglycaemia. Hyperglycaemia stimulates the pancreas, causing an overproduction of insulin. This leads to hyperinsulinemia and a decrease in the number of insulin receptors.
These conditions put the pancreas in a state of chronic 'overload' and eventually lead to islet failure. Histological examination reveals amyloid deposits in the islets.
3. Clinical symptoms
The clinical symptoms of diabetes mellitus are usually polyuria, thirst, bulimia and weight loss. In ketoacidosis, there is anorexia, vomiting, dehydration, exhalation of ketone gas and, in severe cases, coma and even death.

4. Changes in biochemical indicators
4.1 Changes in biochemical indicators due to diabetes mellitus
The common pathogenesis of diabetes mellitus is insulin resistance (IR) and impaired pancreatic β-cell function. Insulin plays a key role in regulating the body's glucose homeostasis. The onset and progression of diabetes is closely related to the biochemical markers in the blood of the affected animals. Therefore, biochemical tests can be used as an important test for the diagnosis of diabetes mellitus.
In addition, diabetes is an endocrine disorder. This can lead to disturbances in lipid metabolism in the affected animals, affecting the levels of triglycerides (TG), lipase (LPS), amylase (AMY), alanine aminotransferase (ALT) and aspartate aminotransferase (AST) in cats. Therefore, the testing of blood glucose and lipids in diabetic dogs and cats has strong clinical significance.
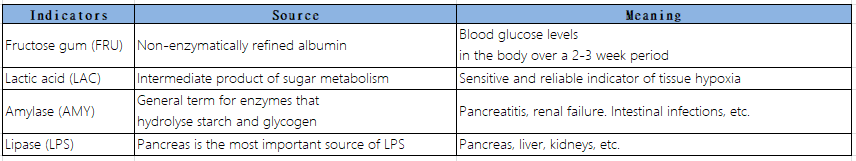
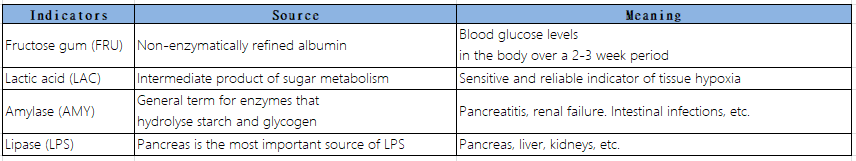
Interpretation of some indicators
4.2 Case analysis
4.2.1 Reason for consultation
The cat presented to the clinic with vomiting and clinical signs of excessive drinking, progressive wasting and urinary leakage.
4.2.2 Past medical history
Chronic valvular heart disease
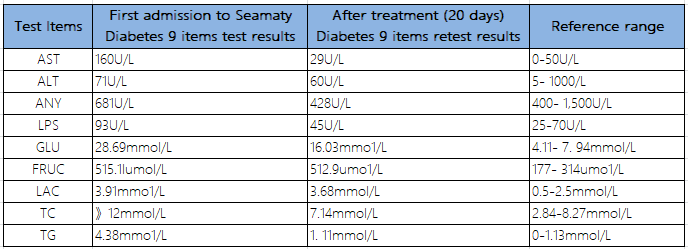
4.2.3 Comparison of index results before and after treatment with Seamaty Diabetes 9 biochemical reagent discs
△Comparison of results before and after treatment with Seamaty Diabetes 9 Biochemical Kit
5. Summary
Long-term ideal control of blood glucose in diabetic animals can help prevent or delay the onset of complications. Fructosamine (FRUC) is formed by a non-enzymatic reaction between albumin and glucose. The half-life of albumin is about 20 days. Compared to glucose (GLU), it can be used as a blood glucose monitor to avoid bias in clinical judgement due to stressful blood glucose changes.
In addition, prolonged hyperglycaemia can lead to disturbances in intracellular enzyme, lipid and protein metabolism in the affected animal. This is a major cause of chronic complications of diabetes.
There are many different diseases that can cause an increase in blood glucose in animals, such as adrenal problems, hyperadrenocorticism and pancreatitis. Monitoring the glucose level in the blood changes all the time and there are also many hormones that affect it, and there are many hormones that raise sugar.
But the only one that lowers sugar is insulin. For example: insulin and glucagon, both located in the pancreas, are secreted. When pancreatitis occurs in animals, insulin secretion is impaired and insulin is reduced, causing the blood sugar to rise. At the same time the leakage of pancreatic enzymes leads to an increase in the secretion of lipase, which in turn secretes fat into fatty acids. The fatty acids chelate with free calcium in the blood, leading to a decrease in blood calcium.
Lactate is an intermediate product of the body's glucose metabolism and can be used as a sensitive indicator in response to tissue hypoxia. In diabetes, insulin deficiency, reduced mitochondrial use of pyruvate and increased glycolysis lead to an increase in lactate. The lack of insulin causes the body to be unable to use glucose to supply the body with energy and instead consumes large amounts of protein and fat, resulting in ketoacidosis.
Glutathione and glutathione aminotransferase, while diabetes consumes protein and fat, fatty acids are released. The fatty acids enter the bloodstream and accumulate in the liver. In the animal organism (especially in cats), the fatty acid deposits later lead to a fatty liver, which in turn causes leakage of liver enzymes. This translates into lesions in the liver, corresponding to an increase in glutathione and glutamate.
In summary, biochemical testing is a powerful clinical aid in the management of diabetes in dogs and cats, and can be an effective aid to clinical veterinarians in the diagnosis and monitoring of the course of diabetes in cats.