What tests correspond to the blood collection tubes of different colors? Is there any difference between venous blood collection and finger blood collection? Why must I be hungry for blood tests?
Blood testing is often the first stop in a medical checkup program. Have you ever wondered what kind of a journey your blood goes through from the time it is collected to the time you get a test report?
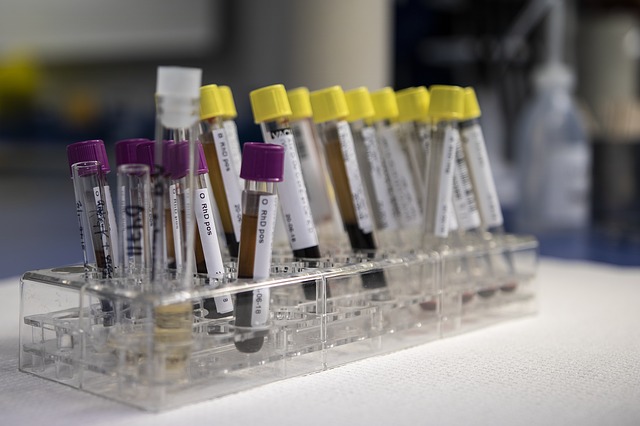
1. The color of the blood collection tube distinguishes the test items
Many people must have seen the different lengths and colors of blood collection tubes behind the laboratory technician when collecting blood. In fact, this is because each container contains different additives, and they are naturally used for different purposes. The nurse will mix the blood collection tubes upside down so that the blood in the tubes is fully combined with the different additives.
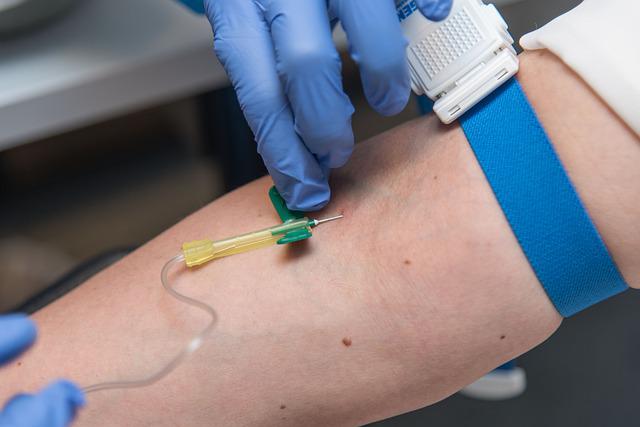
2. There are different blood collection methods
Currently, the main blood collection methods are peripheral blood collection and venous blood collection. Many large hospitals, especially those with a high degree of automation, are now using venous blood for routine blood tests. However, there are still some people who need peripheral blood collection (finger blood, heel blood). For example, in newborns, infants and children, peripheral blood is usually collected for routine blood tests, and the most common method of blood collection is fingertip blood collection.
1) Fingertip blood collection: poor stability of results and obvious pain
Fingertip blood is the peripheral blood of the body, which has poor circulation and is affected by temperature. Especially in winter, blood should be collected after the body, especially the hands, are warmed up, otherwise the results are not stable enough.
Because of the low volume of blood collection or bleeding difficulties, peripheral blood collection often requires a certain amount of pressure, and this action can easily cause tissue fluid to mix with the blood, resulting in abnormal results (increase or decrease) in routine blood measurement.
In addition, it is more volatile and the small amount of blood collected, not easy to review, the inherent error of manual operation and the differences between examiners, are not negligible problems.
The human fingertips are richly distributed with sensory nerve endings, and pain can be more pronounced. Fingertips with wounds, nail infection, redness or skin disease, they should be avoided, another choice to collect finger blood.
With the use of vacuum blood collection system, the volume of blood collected is slightly increased, but it is easy to control the ratio between anticoagulant and blood. With the continuous development of testing technology, the level of automation continues to improve, the human influence factors are reduced, so that the measurement results can be more stable and accurate.
Compared with fingertip blood collection, the nerve endings at the puncture site are much less than those at the fingertip, so the pain during puncture is also less.
3. Non-disease factors affecting test results
The following are common factors that affect test results
1) Gender, race, age and aging, biological rhythm, weight, alcohol, stress, body position, blood collection site, surgery, ionizing radiation, pregnancy, drugs, hemolysis, etc. can affect the test results.
2) Pregnancy: causes high AFP, AMY, cholesterol, triglycerides, low BUN, ALB.
3) Strenuous exercise: CK, CREA, BUN, UA, WBC, K+, BIL, HDL cholesterol will be elevated. LDH, BUN are higher in athletes. Long-term exercise drives up HDL-C, etc.
4) Hemolysis: LDH, BIL, AST, CK, CKMB, AST, MG, K are high. Other minor effects, such as coagulation factors, protein analysis, ALP, P, etc.
4. fasting is the basic respect for the blood test
Before the test, doctors always remind people that they must test on an empty stomach. This is because there are many tests that are affected by food, and the results will not be true if the test is done after a meal.
Eating can cause an increase in glucose, phosphate and bilirubin in the blood. ALT and potassium ions can be significantly higher. Uric acid, protein, calcium ions, and cholesterol are increased moderately to mildly. The level of fat intake determines the level of triglycerides. individuals with O'Lewis-positive blood types can show a significant increase in alkaline phosphatase after eating a fatty meal.
When it comes to the actual diagnosis, a simple breakfast low in fat has no significant effect on the concentration of many blood components. On the other hand, if fat metabolism is to be assessed, a 12-h fast must be maintained. In the past there were strict requirements for fasting to do lipid testing. However, recent expert consensus and recommendations suggest that strict fasting before lipid testing is not necessary.
The difference between fasting and non-fasting is that there is a slight effect on triglycerides, but almost no effect on total cholesterol, HDL cholesterol and LDL cholesterol. For
lipid testing, fasting is still required in China, but there is an increasing international trend towards non-fasting. So if you just want to know your cholesterol level and you can't tolerate fasting, you can do it without fasting. Fasting does not have a significant impact on the cholesterol level.
Fasting for more than 48 hours may cause a more than twofold increase in bilirubin and a decrease in GLU, albumin, C3 and transferrin.
In addition, there are many non-disease factors that can affect the blood tests, which are not listed here.
5. How is the blood sample tested?
After the blood is drawn and mixed, the sample is immediately transported to the hospital's department of laboratory medicine, where the barcode is scanned by a staff member at the sample intake window and the information about the sample owner and the test is transferred to the laboratory's computer. One barcode per tube is never mixed up with anyone else's information.
Different colors of blood collection tubes correspond to different testing items, and samples are received at the reception window in a unified manner and then sorted and processed.
Such as testing biochemical items of the sample is sent to the automated laboratory for testing, the sample into the assembly line, after passing through each position are strictly positioned, passing the need to test the instrument, the orderly addition of samples to test, complete the addition of samples through the sample track and automatically into the refrigerator at the designated location, waiting for the end of each test reaction, the results will be transferred to the computer, pending the doctor's review to ensure that the test results are correct before send a report.
This testing method greatly shortens the test time, and a tube of a barcode identification method also eliminates the phenomenon of data transmission errors.
1) need to centrifuge the blood to separate out the serum or plasma
Tubes containing procoagulant need to be left to stand for 30 minutes to allow the blood to mix well with the procoagulant. Coagulation factors and fibrin are released to shorten the blood clotting time and reduce the clots or fibrin in the serum during the test after centrifugation resulting in needle blockage. This ensures the integrity of the spiked sample, thus improving the accuracy of the test and reducing the test time. In addition, tubes that require centrifugation and contain different anticoagulants (e.g., purple tubes for BNP testing, blue tubes for coagulation testing) need to be centrifuged and tested on the machine promptly after blood is drawn and mixed.
2) Blood that does not require centrifugation
Such as black cap tubes for hematocrit testing and purple cap tubes for routine blood testing, need to be received and promptly sorted on the machine for testing.
6. Why do I have to wait for a long time for blood test results?
For example, hematocrit is the height of blood cell drop in one hour of testing, and if you need to retest, another hour will be added to the original test time.
1) When routine blood tests
When encountering samples from patients with hematologic disorders or platelet aggregation caused by EDTA anticoagulant sensitivity.
When some items of the blood cell analyzer are not classified, or when encountering particularly low platelet values and suspected aggregation, the corresponding rules for retesting should be followed. Smear, staining, microscopy, manual classification, this process takes at least another half hour.
After the blood is drawn and mixed for testing, it is sent to an automated laboratory for assembly line spiking and testing, and finally automatically enters a designated location in the refrigerator where it waits for each test reaction to finish. The test results are automatically transferred to the computer, pending review by the physician to ensure that the test results are correct before issuing the report.
2) When biochemical testing
Problem items or problem samples.
If you suspect that there is a problem with a project or a tube sample, such as the inhalation of fibrous filaments or air bubbles when adding samples, the test results are not produced or reported in error. Through the computer to find and check the designated location of the refrigerator to find the cause, deal with it and then review the results to determine the accuracy of the results, and then give audit and send.
The "traffic jam" during the peak testing period.
A large hospital department of laboratory medicine, just biochemistry laboratory, the daily sample volume can exceed 2,000 tubes, test orders more than 4,000, tens of thousands of test items. Such a huge volume of samples, there is bound to be a rush hour "traffic jam" phenomenon. If you send a test during this time, even if you have a very advanced assembly line, the sample will most likely be blocked in the track. Therefore, choosing the right time to send your test is a good way to ease the pressure of testing and improve the efficiency of reporting, depending on your own medical flow.
7. What do doctors do to ensure blood test results?
Although with the help of automated testing instruments and assembly lines, the physical work of testing physicians is much less. But these instruments also need careful care. They need daily minor maintenance, weekly routine maintenance, monthly major maintenance, but also regular calibration, verification, and indoor quality control every morning and evening. QC is not good to analyze the causes of the project, to find out where the problem, or calibration, or replacement of quality control products, or replacement of detection reagents, or due to system errors re-testing. The final quality control through to ensure that the instrument is operating properly, the test results are accurate.
The test results of the blood testers are finally released through the hospital's LIS software system. People can then print them at the kiosk with their medical record number, or they can check through the hospital's website. Based on the test results, clinicians will make a clear diagnosis and health assessment for everyone.
The workflow of a laboratory technician is intertwined, the fate of the patient is at stake, and every laboratory technician knows the weight of each specimen. Behind it is a life and the expectations of a family. The only thing a laboratory technician can do is to do a good job in every step of the process and to give back the trust of the patients with the fastest and most accurate report. As a patient, you must follow the doctor's instructions and be responsible for your own test results.